or Send Us Your Enquiry

The Thyroid Head and Neck Surgery Centre is a one-stop facility that provides you with a comprehensive evaluation of thyroid nodules, parathyroid disease and head & neck / salivary gland tumours.
An ultrasound is a bed-side non-invasive scan that provides detailed information about nodules arising from the thyroid gland allowing us to distinguish quickly and accurately benign nodules from cancerous ones.
The ultrasound is also very useful in evaluating parathyroid, parotid and salivary gland tumours as well as swollen lymph nodes, neck cysts and other common neck lumps.
This office-based procedure involves the use of the ultrasound to guide a very fine needle precisely into the nodule or lump, from which a small amount of tissue is taken for tissue or histopathologic diagnosis.
The Thyroid Head and Neck Surgery Centre is unique in providing the ultrasound and ultrasound-guided FNAB at the same sitting, with results of the tissue diagnosis usually made available on the same work day.
Computerised Tomography (CT) Scans, Magnetic Resonance Imaging (MRI) and PET-CT Scans are additional scans available in-house that allow us to define and stage cancers accurately, in particular Nasopharyngeal Cancer (NPC) and Squamous Cell Cancer (SCC).
A thyroidectomy, the surgical procedure to remove the thyroid gland, is performed through a curved incision measuring 5 - 8 cm in the lower central neck. It is one of the safest operations performed today, with surgical risks of voice damage or parathyroid dysfunction of less than 1% in experienced hands. It is the most common procedure we perform here at the Thyroid Head & Neck Surgery Centre. Recovery is generally quick; most patients are discharged from hospital after an overnight stay with normal voice, normal swallowing, minimal postoperative pain and complete independent mobility.

Dr Ranjiv Sivanandan is a Specialist Board Certified General Surgeon who has devoted his career to the practice and development of thyroid and head & neck surgery.
After completing his medical degree in Singapore, Dr Ranjiv received his received his advanced training in Head and Neck Surgical Oncology at the Department of Otolaryngology - Head and Neck Surgery at Stanford University, California, USA. Upon completion of the fully accredited program, he was conferred Fellowship with the American Head and Neck Society, and was appointed full-time faculty and Assistant Professor of Surgery at the Department of Otolaryngology - Head and Neck Surgery at Stanford University and the Stanford Cancer Institute until his return to Singapore in 2005.
Dr Ranjiv was extensively involved in scientific research and clinical teaching. He spearheaded research into squamous head and neck cancers at the Stanford Institute of Stem Cell Biology and Regenerative Medicine, and was the first worldwide to publish on Head and Neck Cancer Stem Cells in 2007. He was twice conferred the Resident Teaching Award for the most outstanding contribution to the Residency Program at Stanford University.
Prior to establishing his private practice, Dr Ranjiv was Senior Consultant and Chief of the Head and Neck Service at the Department of Surgery, Singapore General Hospital (SGH), which oversees the largest number of thyroid, parathyroid, parotid and major head and neck surgeries performed in Singapore.
In addition to the numerous thyroid, parathyroid, parotid and major head and neck surgeries he performs every year, Dr Ranjiv has a special interest in the application of robotics in head and neck surgery. In May 2010 Dr Ranjiv performed the first robotic thyroidectomy in Singapore, and in July 2011, the first robotic neck dissection in Southeast Asia. These novel procedures use state-of-the-art robotic technology to remove the thyroid gland and cancerous lymph nodes in the neck without any neck or visible incision.
On a personal level, Dr Ranjiv fervently believes that every condition is unique to the individual, that every patient be informed of best practices and evidence based treatment options, and fully engages patients in the decision making process. He is personally committed to treating the individual not just the disease, and providing the best clinical service and outcome to every patient in his care.
Thyroid nodules and neck lumps are fairly common and the majority are benign in nature. The main cause of concern of a neck lump, however, particularly for an adult, is that it may be the first presentation of a cancer.
Clinical assessment and investigations are geared therefore towards excluding the possibility of an underlying malignancy. You may choose to visit the clinic already prepared with the list of questions that you will like to ask the doctor. It will be helpful if you may also list down any symptoms that you are experiencing such as pain, discomfort, etc.
Your visit with the surgeon should be a comfortable one and normally starts like your visit to a family physician. Effective doctor-patient communication is important to provide quality care and a good surgeon will take time to listen to the patient.
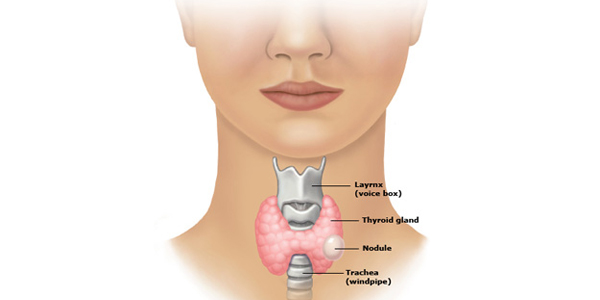
Thyroid nodules are exceedingly common, being clinically detectable by palpation alone in between 4-7% of the general population. Advances in, and increasing use of medical diagnostic imaging has unearthed a much larger reservoir of subclinical nodules (nodules smaller that 1 cm that escape being detected by the patient or the physician). Recent estimates are that about 30% of women under the age of 50, and 50% of women over the age of 60 may have thyroid nodules detectable by ultrasound.
* The main concern with a thyroid nodule is that 1 in 20 harbors a thyroid cancer
Most thyroid nodules present as a painless central neck lump that moves well with swallowing. Nodules are otherwise completely asymptomatic. This applies for both benign and malignant nodules. A lack of symptoms therefore does not assure one is dealing with a benign process. Symptoms of difficulty in swallowing or breathing are sometimes seen in very large nodules. A nodule associated with voice hoarseness, rapid growth, and with other neck lumps should raise the suspicion of cancer.
INDICATIONS FOR SURGERY for a thyroid nodule include:
Thyroid cancer is three times more common in women than in men.
It is the 5th most common cancer amongst women in the United States and the 8th most common cancer amongst Singaporean women. The age standardized rates (ASR) for thyroid cancer in Singapore is 5.8 per 100000.
Although thyroid cancer may not be one of the more common cancers in terms of incidence, it is important for two reasons.
First, thyroid nodules, the most frequent presentation of a thyroid cancer, are very common, and a growing number of subclinical nodules are being serendipitously unearthed by the increasing use of medical imaging.
Second, a little known fact, the incidence of thyroid cancer is increasing at about 7% per year, faster than any other solid organ cancer. The cause for this is not known, but this increase spans across thyroid cancers of all sizes, and therefore cannot be attributed to increased diagnostic scrutiny alone.
There are three main treatment modalities for thyroid cancer.
A robotic thyroidectomy is a novel new procedure that allows for the removal of the thyroid nodule without any neck or visible incision. The incision is placed instead in the under arm.
Our charges for first consultation starts from $200 and our clinic accepts most insurances. In addition, our staff will provide financial counselling for any procedure to be performed.
or Send Us Your Enquiry
Mount Elizabeth Medical Centre
#17-07, 3 Mount Elizabeth
Singapore 228510
Tel: +65 6732 0710
Email: ranjiv@thyroidheadnecksurgery.com
For more details, please visit our main website at www.thyroidheadnecksurgery.com
We are conveniently located at Mount Elizabeth Medical Centre, 3 Mount Elizabeth, #17-07 Singapore 228510.
If you require further directions to our office, please feel free to call us at +65 6732 0710.